You are viewing one section of the Public Health Modernization Toolkit. Please check out the other two sections:
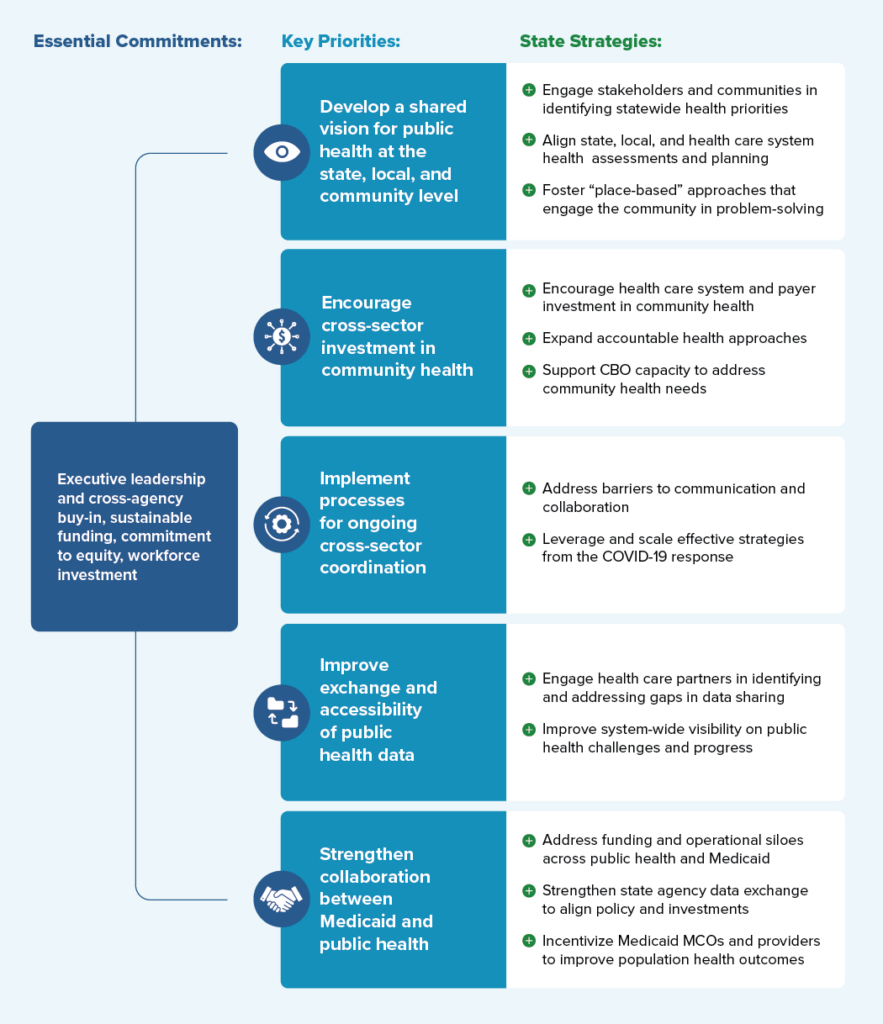
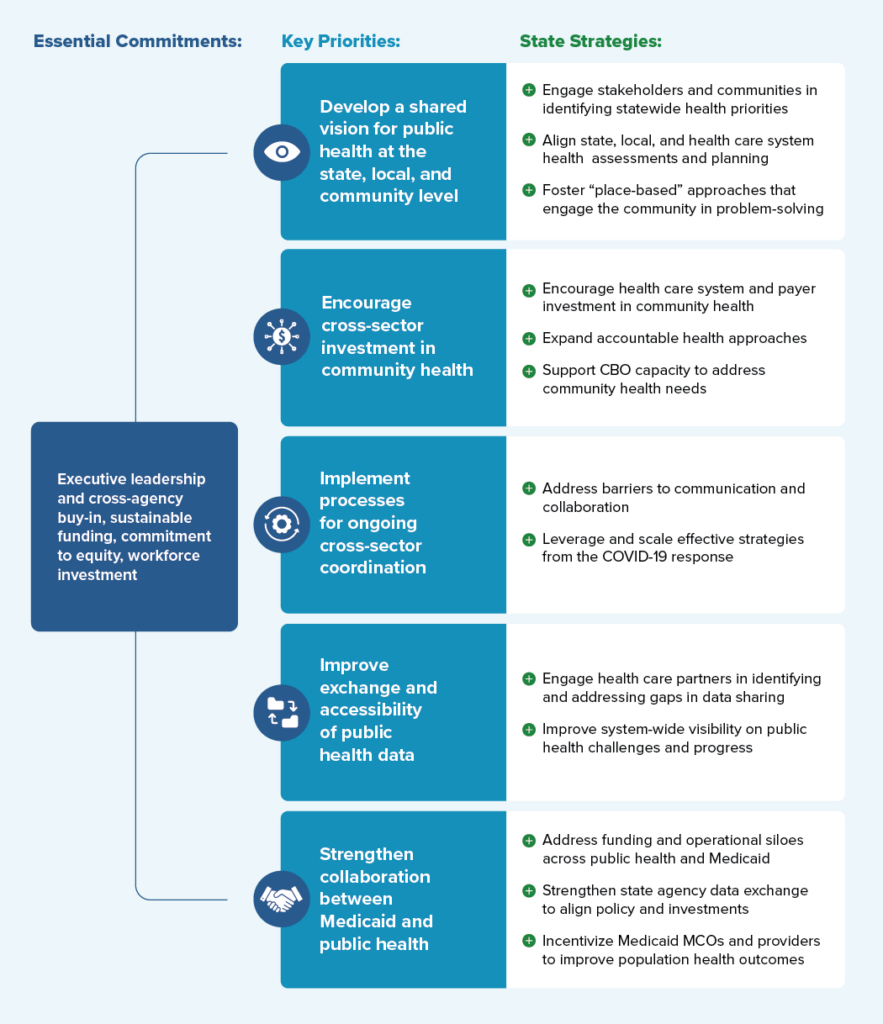
Drawing on interviews with cross-agency state leaders and public health experts, local leaders, and scientific and grey literature, this toolkit provides a framework for understanding essential commitments, key priorities, and policy strategies for fostering collaboration among public, private, and community partners to improve population health outcomes.
Figure 1 displays a consolidated overview of the “Framework for Public Health-Health Care System Collaboration.” Specific examples taken from a variety of states will be examined in greater detail throughout the toolkit.
Robust partnerships between public health and health care systems — capable of sharing information that enables effective population health interventions to stop the spread of disease, increase access to care, or prevent injuries — are a vital part of the public health infrastructure needed to meet community needs. A precondition of sustaining these partnerships is sustained investment in state and local public health capacity. Policymakers and public health experts have widely acknowledged the longstanding challenges in the current public health system stem from both chronic underinvestment and cycles of “panic and neglect” in reaction to public health crisis. Funding for state and local health departments decreased 17 percent between 2009 and 2019, while experts estimate that an additional $4.5 billion per year is necessary to ensure access to basic public health services.[1] On a federal level, experts continue to call for a re-envisioned national public health system supported by sufficient, predictable, and flexible public health funding to support core programming and basic public health capacity.
“Funding for state and local health departments decreased 17 percent between 2009 and 2019, while experts estimate that an additional $4.5 billion per year is necessary to ensure access to basic public health services.”
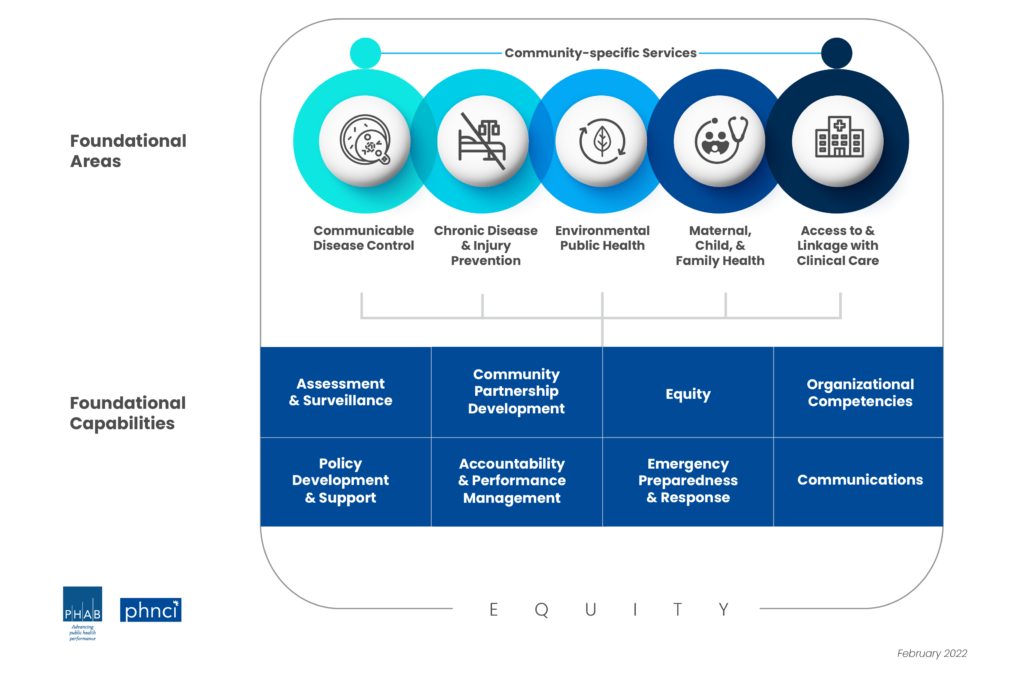
The minimum set of foundational public health capabilities and programs that should be available in every community are defined by the Public Health National Center for Innovations (PHNCI) Foundational Public Health Services (see Figure 3).
On a state level, effective leadership with a sustained commitment to public health is equally important to ensuring that progress and investments made in public health systems in the wake of the COVID-19 pandemic are sustained. According to interviewed state leaders and experts, the following are essential commitments necessary to ensure that effective strategies and bridges built between cross-sector partners can be sustained into the future:

While these essential commitments are a necessary pre-condition to sustain basic public health system capacity, specific priorities and strategies for better engaging healthcare system partners on shared public health priorities are outlined in the sections below.
Public health workforce assessments such as the de Beaumont Foundation and the Public Health National Center for Innovations (PHNCI)’s Staffing Up Initiative and the Public Health Workforce Interests and Needs Survey outline many of the ongoing challenges for the public health workforce, including underinvestment, difficulties in recruiting and retention, and burnout and mental health challenges.
Through the CDC’s Strengthening U.S. Public Health Infrastructure, Workforce, and Data Systems grant program, the CDC will award more than $4 billion to states, localities, and national partners over five years to strengthen public health systems with a focus on workforce, strengthening foundational capabilities, and data modernization. The Association of State and Territorial Health Officials (ASTHO), National Network of Public Health Institutes, and Public Health Accreditation Board, in partnership with NASHP and other public health partners, will provide technical assistance to states and local jurisdictions receiving infrastructure funding.
Additional tools and resources at the national level that states can leverage to support public health workforce include:
Whether states are re-envisioning their public health systems, implementing a State Health Improvement Plan (SHIP), or crafting an interagency approach to a specific health challenge, governors and health agency leadership can help articulate and elevate public health priorities, as well as ensure meaningful engagement processes that promote shared ownership of goals. State leaders play a critical role in convening key internal and external partners, implementing engagement and input processes that foster shared ownership and accountability toward goals at the state and community levels. The following strategies are examples of how states have worked to meaningfully engage partners and communities in developing a “vision” for public health at the state, local, and community level; how states have worked to better align state, local, and health care system-led community assessment and planning efforts; and how states are supporting models for engaging communities in identifying and addressing health priorities.
As outlined in State-Level Examples of Engaging Partners and Impacted Communities in the Development of Public Health Priorities, there are a variety of existing processes at the state level for identifying statewide population and public health priorities, each with their own methods for integrating existing data as well as input and feedback from interested partners and impacted communities. In many states, SHIPs serve as the driving mechanism for engaging health care systems and communities in statewide planning, implementation, and evaluation efforts. Many state and community health planning efforts use the Mobilizing for Action through Planning and Partnerships (MAPP) framework, a strategic planning process that emphasizes broad partner and community engagement, systems change, and the alignment of community resources toward shared goals.
Building in processes for meaningful, culturally informed engagement and ongoing bi-directional communication with diverse partners and impacted communities can help facilitate buy-in and trust and contribute to policies that are more effectively tailored to community needs. Promising examples of processes to engage partners in state health planning and decision-making include:
State Health Improvement Plans (SHIPs): 48 states currently develop their own SHIPs through collaborative, multi-stakeholder processes designed to set the state’s health priorities, target resources, guide programs and policies, and drive collaborative efforts. State health assessments, such as those conducted by Ohio, Alaska, and Pennsylvania, help inform the development of SHIPs and the assessment of progress on state health priorities by providing an overall picture of state health and well-being across key health metrics.
Public health transformation: In states such as Ohio, Oregon, Washington, and Kentucky, public health transformation efforts have driven collaborative processes to define core public health services, assess existing and needed capacity to deliver these services, identify financing and implementation strategies, and define accountability metrics.
Governor and agency-led initiatives: Governors, first spouses, and other statewide leaders have wide authority to elevate key issues and convene partners around common goals. In Indiana, Governor Eric Holcomb charged a Public Health Commission with assessing Indiana’s public health system capacity and developing recommendations for improving capacity, preparedness, equity, and sustainability. Nurture New Jersey, First Lady Tammy Murphy’s office initiative on improving maternal and infant health outcomes, brings together the office, leadership from 18 state agencies, and a broad coalition of maternal and child health partners to reduce maternal and infant mortality, particularly for women of color.
Several states have worked to harness public and private investments in community capacity by aligning hospital community benefit activities with goals identified through SHIPs and Community Health Improvement Plans (CHIPs). Under the Affordable Care Act, the IRS requires nonprofit hospitals to conduct a community health needs assessment (CHNA) and develop a community benefit implementation plan every three years. Such efforts can ensure that community health planning does not occur in silos; that public health, community, and health care systems are all at the decision-making table; and that partners work together to maximize investments. Some key examples of aligning hospital and health care system investment with community needs include:
Communities are typically in the best position to understand and develop solutions to their own health challenges. Partnering with communities can result in increased efforts at a state level to support “place-based” approaches that engage communities in taking a holistic look at community needs and leveraging investments across multiple domains to maximize impact. A collective impact approach provides a model for bringing public health, community members, civic leaders, businesses, health care systems, and other invested partners together to identify community needs and work together toward systems level change. Within a collective impact model, an empowered backbone entity (often a local health department, charitable organization such as United Way, or community-based organizations) plays a central coordinating role in convening and engaging this wide network of community organizations and partners to develop a collectively defined agenda and support ongoing communication, coordination of efforts, measurement, and accountability toward goals.
Such approaches can be powerful tools, helping communities engage with public health and health care system partners to address health concerns and needed interventions such as improving access to high-quality preventive services and addressing social, economic, and environmental factors that affect community health. Although many collective impact models operate on the local or community level, states can play an important role in convening partners, supporting and providing technical assistance to backbone entities, and giving the financial support needed to sustain such approaches.
Innovative approaches such as Health Equity Zones (HEZ) can provide models for empowering place-based, community-led strategies to address community-identified problems and priorities and set the signal for cross-sector collaboration. The Rhode Island Department of Health (RIDOH), in collaboration with state agency and community partners, identified 15 indicators of health equity. A braided funding model, leveraging both categorical public health funding and private and philanthropic investments, allows community collaboratives to have flexibility in identifying and addressing community priorities.
Through dedicated project officers, RIDOH supports community collaboratives with ongoing resources and technical assistance for implementing the HEZ model, including support for the “backbone organization” that manages the ongoing planning, implementation, and financial management of HEZ activities. With Medicaid covering 55 percent of children and 28 percent of adults in Rhode Island, the state is examining strategies to support the scaling and sustainability of HEZs — including aligning with Medicaid and accountable entities approaches with their continued emphasis on braided funding to address health-related social needs and community health. Centering community voices, aligning sectors, and fostering partnerships to support transformational change is also at the heart of the Accountable Communities for Health model (discussed in subsequent sections of this toolkit). Financing mechanisms, including blending and braiding funding streams and accountable health approaches, are often central to bringing together diverse partners and community members to implement and sustain place-based approaches.
The collective impact model has been implemented to address a variety of environmental, educational, and social challenges, and it has also been successfully implemented across jurisdictions to align public health, health systems, business, and community leaders around common population health goals. One example is Live Well San Diego. Through the backbone entity of the County of San Diego, Live Well San Diego aligns cross-sector stakeholders from over 500 organizations, governments, businesses, school districts, and other community partners around a shared vision of helping all San Diego County residents live healthy, safe, and thriving lives. Collectively partners address behaviors, policies, and environmental conditions that contribute to the four diseases (cancer, heart disease and stroke, Type 2 diabetes, lung disease) that account for 50 percent of deaths in San Diego County. Through coordinated efforts to track progress and advance programs and initiatives to improve quality of life in the region, Live Well San Diego was able to drive a 12 percent reduction in the percentage of deaths associated with preventable health threats between 2007 and 2019 among San Diego County residents.